Nothing About Me, Without Me (Including My Health Record): Opening Up Mental Health Clinical Notes
Promote the OpenNotes Movement, Document with Care
〰️〰️〰️〰️〰️〰️〰️
Promote the OpenNotes Movement, Document with Care 〰️〰️〰️〰️〰️〰️〰️
-
OpenNotes is an international movement which advocates for providing patients with access to their electronic clinical documentation and notes, with the purpose of improving transparency and communication in care.
-
OpenNotes has many proven benefits, including:
Strengthening the therapeutic relationship by building trust between the patient and clinician
Improving patient recall and adherence to care plans by giving patients time to review and digest the documented information
Improving accuracy of information within the clinical note by allowing patients to help identify errors and provide feedback
Promoting patient safety and quality of care by encouraging thoughtful documentation that helps maintain efficient workflows and supports whole-person care
Allowing patients to feel more empowered and involved in their care
-
Despite these known benefits, fulsome implementation within Canada remains limited, with patients' access to their clinical notes varying widely by institution.
While some Canadian hospitals have implemented patient portals to provide patients with access to their healthcare information, full access to electronic clinical notes and documentation remains limited and inconsistent, especially in mental health care settings. Even when patients do have electronic access to their clinical documentation through patient portals, notes may be missing, incomplete, or full of complex medical jargon.
The mental healthcare context brings additional challenges, including use of stigmatizing language and concerns among clinicians about the potential for unintended harm or misunderstanding given the sensitive content within these notes.
How to Implement OpenNotes
To support clinicians in adopting and implementing OpenNotes, the Digital Mental Health Lab developed a toolkit alongside 23 mental health clinicians (case managers, nurses, social workers, psychologists, psychiatrists, and residents).
This practical toolkit offers strategies to help clinicians build broader awareness of OpenNotes and strategies to implement person-centred documentation practices in the Canadian psychiatric context.
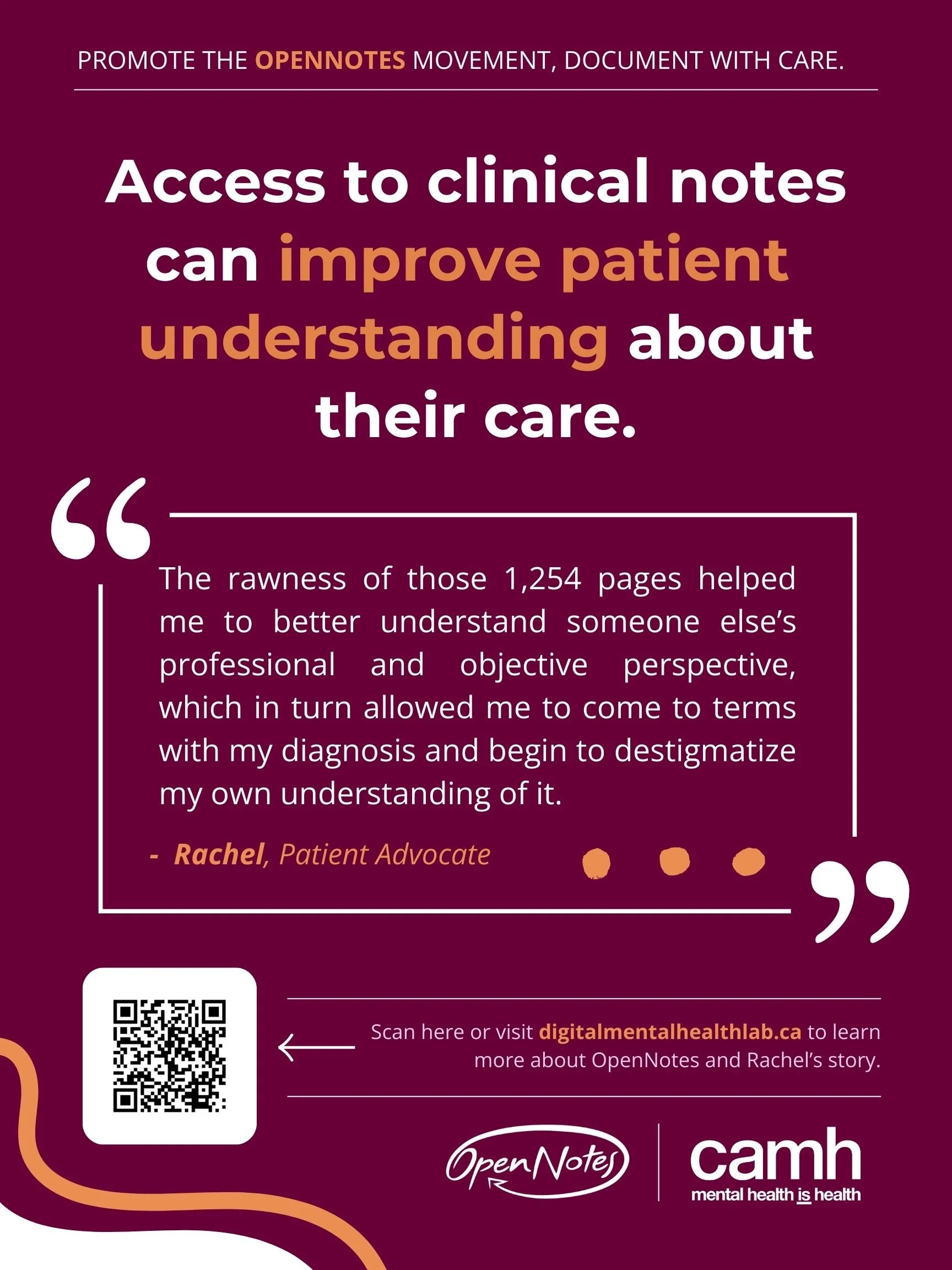
The Impact of OpenNotes: Sharing the Lived Experience
To further encourage clinicians to adopt OpenNotes practices, the Digital Mental Health Lab has collaborated with patient advisors to co-create poster and video testimonials. These testimonials highlight personal stories about how access to their clinical notes has shaped their care experience and what this access means to them.
Continue below to watch their testimonials and read their stories.
By including the patient voice, we aim to demonstrate how OpenNotes can improve patient care and experience, and to encourage clinicians to adopt OpenNotes practices.
The Impact of OpenNotes: Video Series
The Impact of OpenNotes: Written Experiences
In addition to our video series, patient advisors developed written testimonials to share their experience accessing their clinical records. Expand each row below to learn more about each advisor’s experiences.
-
The last time I was inpatient at CAMH I had an excellent and very thorough psychiatrist. [My psychiatrist] wrote detailed discharge notes recommending some post-discharge treatments and tests. I did not know about these notes at the time, and my community psychiatrist never mentioned them to me when I saw him post-discharge. None of the recommendations were implemented. I learned about the notes several years later when I was accessing my CAMH records for another reason and [the discharge notes] were included with them. I asked my community psychiatrist about it, and he said he never received the notes. By that point, the additional treatments that my inpatient doctor had recommended were no longer relevant. I feel that had I had access to the notes at time of discharge, I could have raised it with my community doctor, and I might have benefited from access to additional treatment and testing at the time.
-
Access to my clinical notes gave me a sense of autonomy over my mental health and placed me on a road to recovery that allowed me to learn more about myself than I thought possible. After multiple in-person hospital stays at CAMH, I was able to request and receive my clinical notes through a straightforward process. It felt empowering to have my personal files in my possession and reading through them was an eye-opening experience- both at that time and even now. The rawness of those 1,254 pages helped me to better understand someone else’s professional and objective perspective, which in turn allowed me to come to terms with my diagnosis and begin to destigmatize my own understanding of it. It is important to reflect on ourselves, and records can truly help someone understand their illness and become more aware of the signs and symptoms for the future. There is no harm in getting to know yourself better. Although I couldn’t read all the pages right away, over the years I have gone through the various portions of my file- something that I will have access to for life- and it has created a world of difference for my own understanding of what my episodes look like and why they may look like that. It has helped me to work backwards in understanding myself and most importantly, learning how to forgive myself too.
-
Being a newcomer in Canada, I was unsure of how my data might be used. Even though I was told that the information I share during my therapy sessions will not impact my immigration status, the anxiety lingered. It took some time to receive access to my notes and the task of asking for it was daunting. Because these words were through the eyes of a professional, I was not sure how I would be perceived or how I would feel after reading the notes about myself. The organization and the mental health professionals were kind enough to stay in touch with me while they compiled the notes and ensured that it aligned with their privacy policy. When I finally sat down to read the notes, there was a mental health professional sitting with me to answer any questions I had. It was a relief to see that the notes portrayed the truth. I was also surprised to read the non-judgmental tone. Things that I wouldn't have noticed about myself were observed and documented. It gave me an insight into what my therapist thought of me and how compassionate they were. This gave me the reassurance I needed. It gave me confirmation that the organization and professionals were acting in my best interest. Although this might be obvious in most cases, for me, it wasn't. I'm grateful to have had access to my clinical records. It helped me feel empowered.
-
I've found that being able to view my clinical notes is crucial to getting proper healthcare. Often, I'll read my clinical notes and find that my doctor has written something entirely different in the notes than what they've communicated with me. I've found diagnoses in there that were not shared with me, accounts of appointments that don't match my experience at all, and errors made under anesthesia that I was not informed of. I also have found very biased, judgmental descriptions. I realize that in mental health care especially, a person's demeanour, style of dress, and overall comportment are useful information for diagnosis. However, sometimes these descriptions [in the clinical note] seem to veer outside the strictly helpful and diagnostic and enter the realm of personal judgement. I believe that patients should be permitted to contribute their own account of an appointment, treatment, or procedure to the record - it scares me that so many of these inaccurate notes doctors’ have written about me will be taken as gospel by the next one who sees me.
-
As a patient here at CAMH, for the first time in my life I was willing to talk about myself and what I had been going through. I kept on repeating throughout treatment that here’s a group of people, my care team, that is working so hard. They were quite heartened by the fact that I was making progress. I was taking notes with all the interactions that I had. I wanted to go back and if we had forgotten something, to bring it up. And if they mentioned something, at least I would have a recall and that would be through our notes. Whatever I said was valid. I wasn’t belittled. Every point was taken down. And that creates a picture of yourself. Access to my clinical notes gave me a sense of autonomy over my mental health and placed me on a road to recovery that allowed me to learn more about myself than I thought possible. While reading through my notes, I realized how much attention was being paid to me. It might come across as something very tertiary and nothing to do with the treatment, but it’s written down. It makes them understand you and you understand them.
As a clinical professional, you stop communicating with the outside world. You are using these medical, biological terms — they don’t make sense to anybody else except clinicians. And when you are using that language you are not communicating. Information is not being relayed, it is getting lost. Do away with jargon. Talk to people in everyday, simple terms. I started to teach Health Sciences students, about 12 different professions, at the University of Toronto. It’s inter-professional education and we bring in the aspect of patient-oriented care; where the patient is at the centre and the care team is built around them. My part is to instruct the students as to how important it is to listen to the patient, understand them, and to bring in humility. When you talk to someone, their guard goes down and they’re willing to share what they are feeling, which will help in treating patients and looking after their welfare. Now you are on an equal footing. And that’s what I want to bring to my students. There is no hierarchy, information travels laterally, and you share; no matter what background. When you start to do that, patients will start to become more forthcoming. When you have everything that you need to come up with a treatment plan, it makes it a lot easier.
-
Before I had access to my notes, I often left appointments feeling overwhelmed and unsure of what had actually happened and what we discussed. Living with multiple complex and chronic conditions means that every visit matters—and yet, with only 15 minutes to cover everything, there was rarely time to unpack the complicated medical jargon or revisit what was said. I’d try to remember the terminology, go home, and Google what I thought I heard—but it was a guessing game, and I always felt a step behind and was left more confused about my body, my care and next steps.
I first learned that I could read my notes when a care provider encouraged me to check the patient portal. At first, I was nervous—would I even understand what I was reading? Would this complicate things even more? But when reading my notes after a visit, I felt empowered. And this was a missing piece. I could finally see the full picture—not just what I thought was said out loud, but how my doctor interpreted things, what they were thinking, and what came next. Being able to review my notes gave me the chance to research the often confusing medical terms, reflect on next steps, and come to my next appointment more prepared. It reduced my anxiety and helped me feel like a true partner in my care. I could ask better questions, explore treatment options I had learned of, and felt more in control of what was happening to me. It’s important to know that having access to notes doesn’t challenge your role as a clinician—it enhances it. When patients are informed, they can collaborate. Especially in complicated medical cases, access to notes can be the bridge between confusion and clarity, between fear and empowerment. Nothing about me, without me—including what’s written about me. That’s what OpenNotes means to me.
-
Having access to my medical records has changed the way I navigate my healthcare. For the first time, I could see what was being written about me, what decisions were being made, and where things didn't add up. This gave me a sense of agency, but it also showed me something harder to face; that mistakes and oversights in my care had often gone unnoticed until after the harm already occurred. Accessing my records has been empowering, but it hasn't been easy. Anytime I would point out a discrepancy, I could feel the dynamic with my provider's shift. Instead of open conversation, I felt a wall go up. My questions were treated like challenges rather than part of my care. That makes it harder for them to take accountability and harder for me to feel safe in sharing my concerns. Over time, this has fractured my relationship with my providers. Trust breaks down communication suffers, and I am left carrying that weight.
The phrase “nothing about us without us” really speaks to my experience and I'll give an example. After an emergency room visit, I had followed up with my family doctor and told them what happened. They just told me that I was wrong and what I was describing didn't occur. But I knew what I'd been told and I knew my own experience. The only way I could prove it was to request the records myself. That came at a cost to me financially and emotionally. I had the money to pay, but I shouldn't have had to spend it just to access information about my own healthcare. And when the records finally did come, they confirmed exactly what I had said all along. My doctor had already had this information, but somewhere along the line, the truth got dismissed. By then the damage was done. Trust was lost, I had already been denied the care I needed, and there was no way to undo that harm. This should never be the reality and I shouldn't have to choose between paying for records or staying silent. I shouldn't have to sit at home researching medical terms and piece them together like a puzzle just to understand my own health care. And I shouldn't have to prove myself right in order to be taken seriously. Yet this is what I've been forced to do time and time again, and I know I'm not alone. If records were free, open and part of regular care, things would be different. If providers and patients looked at the same information together in real-time, it would build trust instead of breaking it. It would prevent harm. It would create accountability and it would allow patients like me to feel heard instead of feeling like we have to fight every step of the way or avoid care altogether because of a history of being dismissed, not believed or being treated less than. To me, this is more than paperwork. It's about safety and it's about dignity, and it's about my life. I shouldn't have to fight for access to my own healthcare and no one else should have to either.
-
I don’t get access to electronic client notes in regards to my mental health often, but I have been deeply affected by the stigma and judgement I have read in these notes when I have had access. For example, I have read that I am “manipulative,” which i feel was stated solely because of the stigma they held about my past drug using history. Rather than looking through a trauma informed lens, I was viewed as manipulative rather than seen as engaging in survival-based coping behaviours to meet my basic needs. I read phrases like “she claimed”, which suggests to me that I was not believed in my “claims”. However, this was my lived experience that was shared. Not a claim. This was my truthful perspective. This amplifies my own, internal self-stigma.
Clinical records should be leveraged. Organizations need to advocate for more training of mental health care clinicians to reduce stigma and put pressure on clinicians to make necessary changes that will lead to better health outcomes.
Be an Advocate
We need you! Help us spread the word and advocate for OpenNotes.
Share these poster testimonials within your own organization to encourage healthcare professionals to adopt proper clinical documentation skills and showcase the impact OpenNotes has on patient experiences.
-
OpenNotes. (2023). https://www.opennotes.org
Kassam, I., Shin, H. D., Durocher, K., et al. (2022). “I think it’s something that we should lean in to”: The use of OpenNotes in Canadian psychiatric care contexts by clinicians. Digital Health, 8, 20552076221144106. https://doi.org/10.1177/20552076221144106.
Bourgeois, F., Lowe E., & Wachenheim, D. (2018). OpenNotes: Sharing visit notes with patients and families. Pediatric Nursing, 44(1), 45-48.
Mishra, V. K., Hoyt, R. E., Wolver, S. E., et al. (2019). Qualitative and quantitative analysis of patients’ perceptions of the patient portal experience with OpenNotes. Applied Clinical Informatics, 10(01), 010-018. https://doi.org/10.1055/s-0038-1676588
Nazi, K. M., Turvey, C. L., Klein, D. M., Hogan, T. P., & Woods, S.S. (2015). VA OpenNotes: exploring the experiences of early patient adopters with access to clinical notes. Journal of the American Medical Informatics Association, 22(2), 380-389. https://doi.org/10.1136/amiajnl-2014-003144
Bell, S. K., Mejilla, R., Anselmo, M., et al. (2017). When doctors share visit notes with patients: a study of patient and doctor perceptions of documentation errors, safety opportunities and the patient-doctor relationship. BMJ Quality & Safety, 26(4), 262-270. https://doi.org/10.1136/bmjqs-2015-004697
Esch, T., Mejilla, R., Anselmo, M., et al. (2016). Engaging patients through open notes: an evaluation using mixed methods. BMJ Open, 6(1), e010034. https://doi.org/10.1136/bmjopen-2015-010034
Petersson, L., & Erlingsdóttir, G. (2018). Open notes in Swedish psychiatric care (Part 1): survey among psychiatric care professionals. JMIR MH, 5(1), e9140. https://doi.org/10.2196/mental.9140
Schwarz, J., Bärkås, A., Blease, C., et al. (2021). Sharing clinical notes and electronic health records with people affected by mental health conditions: scoping review. JMIR MH, 8(12), e34170. https://doi.org/10.2196/34170
Blease, C., Kharko, A., Hägglund, M., et al. (2021). The benefits and harms of open notes in mental health: A Delphi survey of international experts. Plos One, 16(10), e0258056. https://doi.org/10.1371/journal.pone.0258056
Acknowledgement of Support
Funding is provided by the Ontario SPOR SUPPORT Unit, which is supported by the Canadian Institutes of Health Research, the Province of Ontario and partner Ontario hospital foundations and institutes.
Contact Us
Please reach out below if you have questions, want to learn more, or would like our team to present to your organization about OpenNotes.